What is clinical governance?
The quality and integrity of clinical care is one of the most strictly regulated facets of healthcare. A robust clinical governance model is now a crucial and unavoidable requirement for the modern healthcare provider. So, what is clinical governance? And how can healthcare quality professionals embed it?
Clinical governance meaning
Clinical governance is a framework of accountability for NHS healthcare organisations in the UK. It focuses on continual improvement and always ensuring a high quality of care.
We’re all familiar with the important role of governance, in tandem with risk management and compliance, in shaping how organisational processes deliver optimal outputs for customers and stakeholders. Financial governance, for instance, has been around in some form since the 1950s. Yet surprisingly, it wasn’t until 1998 that the NHS in the UK began to adopt a unified governance framework for guaranteeing and continuously improving clinical quality.
Clinical governance is the culmination of this focus on sharpening and continuously optimising the quality of healthcare. In short, an effective clinical governance model should give your healthcare organisation a framework that lets you:
1. Safeguard and maintain the levels of care you provide to patients
2. Measure and continuously improve operational quality levels
3. Build an environment where controlled change management and stakeholder involvement can drive optimised clinical care
Although clinical governance emerged as a way to standardise and improve public healthcare and is used almost exclusively in the UK to refer to NHS practices, its principles can be applied to any public or private healthcare provider that offers clinical care.
The 7 pillars of clinical governance
7 core components, or ‘pillars’, should feed into your clinical governance model. These are:
1. Clinical effectiveness & research
The core of your clinical governance initiative. Is your organisation doing what it should to treat patients effectively? Guaranteeing the efficacy of your clinical practice means:
- Staying up-to-date with new standards, guidelines, studies and models as they emerge by keeping abreast of the latest research and regulations
- Establishing a mechanism for measuring the levels of care and satisfaction you provide
- Using those measurements and other evidence to inform future care
2. Risk management
Like any business, your clinical operation should be able to measure, manage and control your risk environment. That means you should have a system for:
- Reporting risks, incidents and near-misses quickly and easily
- Scoring and treating risks with targeted controls
- Harnessing improvement suggestions and opportunities for a proactive quality improvement approach
3. Patient & public experience & involvement
As a model developed for public healthcare, clinical governance should take into account the experience of your patients and the wider public – and use feedback to tweak and amend your clinical practices in a patient-centric way. Consider how to maximise patient and public involvement with initiatives such as:
- Surveys and questionnaires
- Forums
- Patient representatives on your hospital/practice board
4. Auditing
Clinical practices are like any other operation: deep, targeted auditing is vital for uncovering risks and pinpointing improvement opportunities. Manual, paper-based processes are increasingly unable to adequately and time-effectively give clinical auditors this information, so consider how to embrace the latest auditing technology.
The benefits of modern digital auditing include:
- Instant post-audit report generation, saving days of effort each month
- Bespoke question banks and checklists for a consistent but flexible approach
- Multi-device capability for mobile, paperless auditing of any nook and cranny of your clinical practice
5. Staff management
Your clinical staff are vital enablers of your governance framework. Staffing issues, untrained workers and undermotivated staff are all critical threats to the integrity of your clinical quality. Robust workforce management should include:
- Building an open culture for raising and resolving issues and concerns
- Establishing a mechanism for measuring and maximising staff input and performance
- Ensuring that your recruitment and long-term management strategies are aligned with your clinical governance goals and objectives
This leads into…
6. Training
Continuous clinical quality improvement is impossible without effective training, upskilling and continuous professional development (CPD). Think about how to implement practices such as:
- Encouraging relevant staff to research current and upcoming developments and trends, perhaps by attending conferences and courses (see Pillar #1!)
- Regular feedback and appraisal sessions
- Structured and collaborative training pathways for each member of staff
7. Information
Controlled, consistent information is vital for effective clinical governance. In particular, you should think about:
- How documents are controlled and shared (or not!) across your organisation
- How information security and data protection standards like ISO 27001 and the GDPR can be baked into your information management processes for a ‘privacy by design’ approach
- How you can have confidence that your data meets ALCOA+ principles
- How as much data as possible can be fed into your clinical governance model to inform future best practice
And you shouldn’t just consider patient data here. Strong information management should support all 6 of the other clinical governance pillars. So, it’s crucial that you have a centralised and effectivedocument management system that gives relevant staff quick, easy and secure access to:
- Operational day-to-day documents like SOPs and policies
- Training records
- Audit data and findings
- Risk registers and scores
- Relevant documents like new NICE guidelines or National Service Frameworks
Culture and leadership
The 7 pillars of clinical governance are a good way to ensure you’re covering the main bases of a functional clinical governance approach. But they aren’t an exhaustive list of requirements. In particular, it’s important you also have a supportive culture with strong leadership underpinning your clinical governance initiatives.
A designated senior clinician should be in place to offer oversight and guidance, and to foster an open quality-focused culture where mistakes, research, trends and best practice can be candidly shared. As in ISO 9001 Clause 5, clinical leadership should demonstrate commitment to, and involvement with, continuous quality improvement: quality and governance issues should be raised in frequent board-level discussions, and clear improvement objectives mapped out at all levels of your operation.
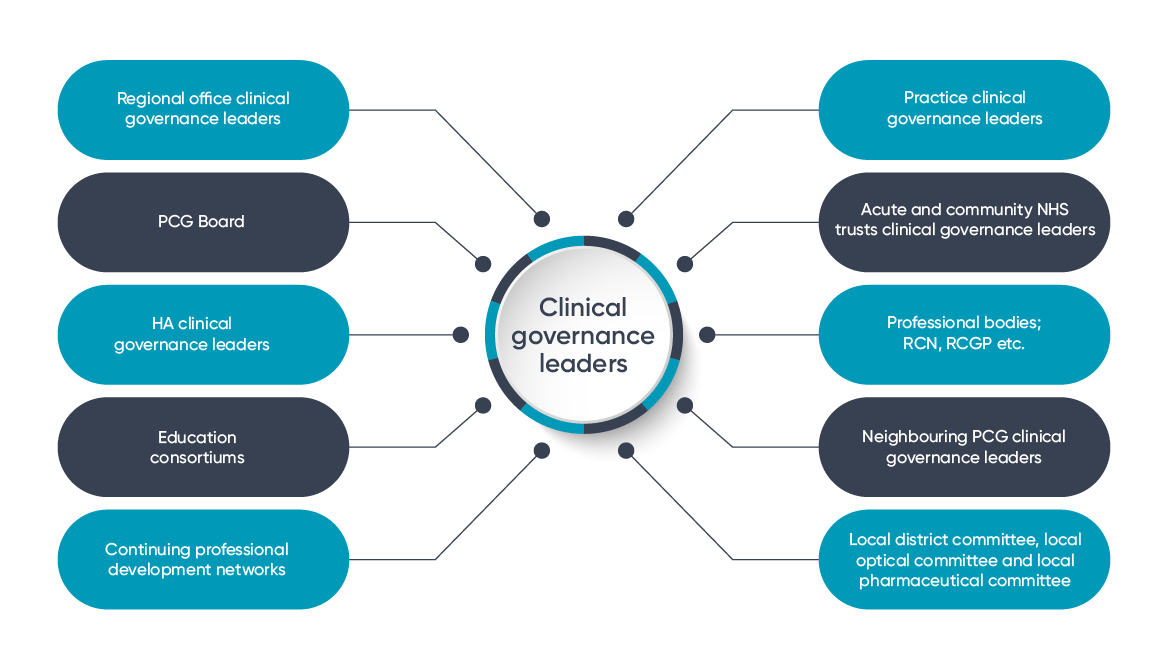
Clear focus on stakeholder involvement should be supported by a centralised quality management system – particularly one which makes the sharing of clinical and quality data as visible and simple as possible. Consider each stakeholder who might support and strengthen your clinical governance model, and ensure they’re included.
Examples could be:
Aaron is an experienced content writer specializing in quality and compliance, with a focus on regulatory standards and enhancing operational practices. With a strong background in the life sciences and manufacturing industries, he excels at creating clear, impactful content that supports organizations in achieving sustainable excellence and meeting complex industry requirements.


